Exploring the Role of Gut Inflammation in Depression
Addressing gut health can have a profound impact on brain function, depression, mood, energy levels, and motivation—factors that antidepressants don’t address.
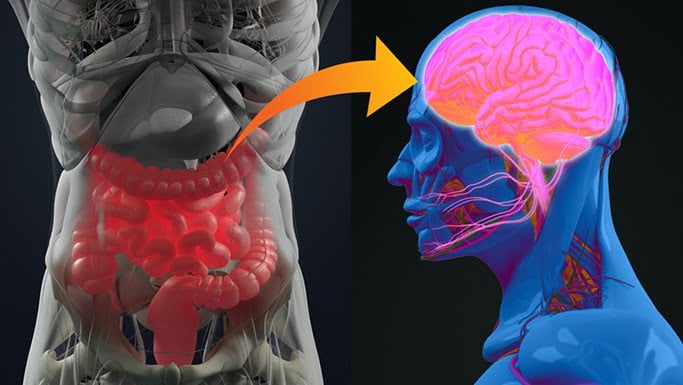
The gut-brain connection.
By Datis Kharrazian 12/25/2023
Depression isn’t an antidepressant deficiency. In fact, for many people, the problem may stem from inflammation in their gut. For the estimated 40 percent of Americans complaining of one or more gut symptoms, depression may be one of them.
Studies have found that the inflammatory signals released in the gut can travel to the brain, affecting brain function and possibly triggering depression. Clinically, I’ve seen many patients resolve their depression simply by dampening gut inflammation.
The Relevance of Gut Inflammation in Depression Today
Depression affects more than 264 million people worldwide, making it a leading cause of disability. Its impact extends beyond the individual to families, communities, and society as a whole.
Depression isn’t the only fallout from poor gut health. Gut health has been associated with various other physical and mental health conditions, including anxiety, stress, poor immune resilience, and even neurodegenerative diseases such as Alzheimer’s.
Depression is a red flag, a warning that something is amiss and needs urgent attention. All too often, it’s gut inflammation because of modern diets, excess sugar or alcohol consumption, food sensitivities, gut microbiome imbalances, and chronic infection—all of which inflame the gut.
Mechanisms of Gut Inflammation and Depression
The bidirectional communication between the gut and the brain is known as the gut-brain axis. It plays a crucial role in depression.
Inflammation in the gut sends signals to the brain through various pathways, disrupting the brain’s normal function. One key mechanism is the release of inflammatory molecules, such as cytokines, which cross the blood-brain barrier. Once in the brain, they disrupt the delicate balance of neurotransmitters, such as serotonin, dopamine, and norepinephrine, crucial for regulating mood and emotions.
Studies have shown that increased levels of pro-inflammatory cytokines, such as interleukin-6 and tumor necrosis factor-alpha, are associated with depressive symptoms.
These cytokines also inflame the brain itself, slowing conduction between nerves. This slowed nerve conduction can cause symptoms such as brain fog, depression, fatigue, and loss of motivation.
The Role of ‘Leaky Gut’ in Depression
Intestinal permeability, also known as leaky gut, is a condition in which the gut lining becomes compromised, allowing substances to leak into the bloodstream. This can occur because of unhealthy gut bacteria, poor dietary choices, food sensitivities, and chronic inflammation. Leaky gut has been implicated in many health conditions, including depression,autoimmunity, and poor immune resilience.
When the gut barrier is compromised, harmful substances, such as bacterial toxins and undigested food particles, enter the bloodstream. These substances trigger an immune response, leading to systemic inflammation. In turn, this inflammation can affect the brain, contributing to depressive symptoms.
The Influence of the Blood-Brain Barrier on Depression
The blood-brain barrier is a protective barrier that separates the bloodstream from the brain. Its primary function is to regulate the passage of substances into the brain, allowing in essential nutrients while keeping out harmful compounds. However, in conditions such as leaky gut, the integrity of the blood-brain barrier becomes compromised. In other words, leaky gut is often accompanied by “leaky brain.”
When the gut is inflamed and leaky, compounds that would typically be prevented from crossing the blood-brain barrier can enter the brain. These compounds activate immune cells in the brain called glial cells, leading to brain inflammation, worsened brain function, and depression.
The Role of Blood Sugar Regulation Pathways in Depression
Research suggests that imbalances in blood sugar levels can contribute to depressive symptoms. The gut plays a crucial role in regulating blood sugar levels by releasing gut peptides, such as glucagon-like peptide 1.
Clinically, we commonly see blood sugar imbalances as a major contributor to depression and other mood disorders. Tolerance for carbohydrates varies from person to person, depending on fasting blood sugar and insulin levels, levels of physical activity, and other factors. But for most Americans, cutting out sugar and processed carbohydrates can have profound impacts on both gut health and mood.
Blood sugar imbalances can also stem from gut dysbiosis (an overgrowth of bad gut bacteria), affecting energy levels, mood stability, and overall mental well-being.
Gluten Intolerance and Depression
Some people’s mood disorders are simply caused by an intolerance to gluten, the protein found in wheat and wheat-like grains. Gluten can be highly inflammatory to both the gut and the brain in those with an immune sensitivity to it. Some gluten-sensitive people won’t have any gut symptoms at all but will express a gluten intolerance neurologically through mood or cognitive disorders.
For others, the chronic gut inflammation caused by gluten will inflame the brain. Either way, simply going gluten-free in these individuals can profoundly reduce inflammation and hence symptoms of depression.
Fixing the Gut: More Than Just Taking a Probiotic
Animal studies have shown that different strains of probiotics can influence mood and behavior. These findings suggest that the gut microbiome plays a role in mental health.
While some may see relief from depression by taking probiotics, many won’t. The complexity of the gut microbiome and its interaction with the brain is more complex than that.
Instead, what’s more often required is an inflammatory overhaul to remove inflammatory triggers from the diet, stabilize blood sugar, manage any chronic infections, and shore up other areas of imbalance.
As in most areas of health, dampening gut inflammation isn’t a “one-and-done” approach with a drug or supplement, but rather is part of a multi-variable health protocol.
Addressing Depression Through Improved Gut Health
While I’ve covered various ways in which poor gut health can promote depression, this isn’t to suggest that it’s the only mechanism. Undiagnosed or poorly managed autoimmune conditions, hypothyroidism, chronic infections, hormonal imbalances, or past brain injury are examples of other factors that can contribute to depression and require different approaches to management.
What’s more, a sedentary lifestyle and junk food diet play significant roles in depression. Multiple studies have shown that exercise alone can alleviate depression.
Exercise supports the brain in several ways that can help to prevent depression, such as by promoting nerve cell growth, stimulating the release of mood-boosting chemicals, regulating neurotransmitters, reducing stress, and improving sleep.
Nevertheless, the gut plays an important role in brain health.
Clinical strategies to dampen gut inflammation and improve gut health include:
- Adopting a whole-foods diet similar to what our pre-industrial ancestors ate.
- Identifying and addressing food sensitivities.
- Improving gut microbiome health and diversity.
- Addressing leaky gut (intestinal permeability).
- Testing for and addressing common gut infections, such as H. pylori, candida, parasites, and small intestinal bacterial overgrowth.
- Addressing breakdowns and disorders in the digestive tract, such as gastric ulcers, insufficient stomach acid, poor gallbladder function, insufficient pancreatic enzyme release, leaky gut, poor motility, and potential gastrointestinal autoimmunity.
These topics are beyond the scope of this article, but if you visit my YouTube channel or website, I offer plenty of free content on improving gut health.
Addressing gut inflammation, restoring gut barrier integrity, rebalancing the gut microbiome, and adopting personalized gut-healing approaches can have profound impacts on brain function, depression relief, mood improvement, and energy and motivation boosting—factors that antidepressants don’t address.

